As we continue to address health inequities, understanding how algorithms impact races differently is important. One of these inequities revolves around the racial disparities in kidney disease, with Black individuals experiencing a 2-to-4-fold higher incidence of kidney failure than White individuals. Moreover, Black individuals have faced lower referral rates for pre-dialysis transplant evaluation, post-kidney failure transplants, and placement on transplant waitlists. One contributing factor to these disparities is the guideline-recommended estimated glomerular filtration rate or eGFR. Simply put, this measures how well the kidneys are filtering, which, unfortunately, has been found to overestimate kidney function by up to 21% in Black individuals. Consequently, a Black individual’s kidney function is inaccurately assessed as better than it genuinely is, leading to delayed treatment and missed opportunities for kidney transplantation. This discrepancy in the eGFR resulted in an estimated median delay of 1.9 years in Black individuals meeting thresholds for certain levels of care compared to White counterparts.
This is unacceptable.
Recognizing the need for change, the American Society of Nephrology (ASN) and the National Kidney Foundation (NKF) have recommended adopting a new race-free equation to estimate kidney function accurately. This significant recommendation paves the way for more equitable clinical practices and improved health outcomes for all individuals, regardless of race. Additionally, the US Organ Procurement and Transplantation Network (OPTN) has recently changed its methodology for determining organ allocation. This proactive step by the OPTN highlights its commitment to addressing algorithmic biases in kidney transplantation.
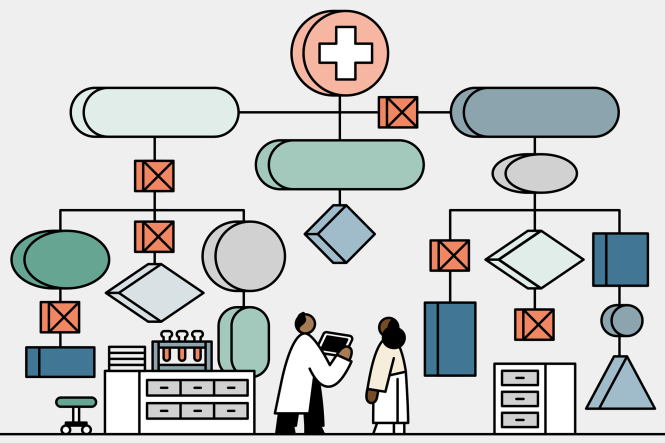
Achieving meaningful change in healthcare requires the collaboration of three essential components:
- Identifying flawed algorithms
- Revising guidelines by professional organizations
- Implementing adaptive measures by regulatory bodies
This multifaceted approach recognizes that while there may be instances where differences based on race are necessary, there are also situations where these differences can create harm. To effectuate change, fostering open and transparent endeavors to study, reassess, and adjust our thinking is crucial. However, changing clinical behaviors poses challenges. It requires a concerted effort from laboratories to modify how they calculate and report results. End users, including healthcare professionals, must understand the rationale behind the change and the scientific evidence supporting it, subsequently adapting their treatment approaches accordingly.
Addressing health inequities in kidney disease care demands an active commitment to combating algorithmic biases. By acknowledging and rectifying flaws in eGFR guidelines, professional organizations, and regulatory bodies are taking significant steps toward promoting algorithmic fairness. However, sustaining progress requires ongoing research, transparency, and collective efforts from the healthcare community. Let us embrace a process that fosters open-mindedness, adaptability, and collaboration to create meaningful change for the betterment of all individuals we serve.
