
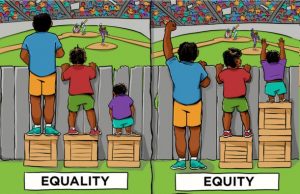
One of my favorite images is a picture of three boys standing behind a fence trying to watch a baseball game. One is tall enough to gaze over the fence; the other two are of different heights, and unable to glimpse the action. There are three boxes stacked next to them. The question posed is “How would you distribute the boxes to help all the boys watch the game?” It is not meant to trick you, although it is imperative to ask; it is one of defining equity versus equality. The problem concerns all three boys being able to look over the fence. If you distribute the boxes equally, one for each on which to stand, the taller boy has not gained anything; the middle sized is now able to peek over the fence and the shortest is not any better off, even though he is utilizing the box, he still can’t see over the fence. However, if we adjust our perspective to equity, the tallest boy will not receive a box, as it is unnecessary, the subsequent middle one would still receive one box on which to stand, and the shortest would peer over the fence by standing on the remaining two boxes, thus all three are now able to see the game.
Since basic healthcare is an innate right for all, its distribution is crucial. If the goal is to aid as many as possible to receive a level of care that is appropriate and equitable, we must consider not only their clinical disease state but also their socioeconomic status (SES), since it plays such an essential role in their well-being. Risk based payment adjustments relate to the degree of illness and co-morbid conditions. However, none adjusts for their SES, as all are not equal in that dimension. With the needs of those we serve being different based on their socioeconomic status, considering these factors will move us from a model of equality to one of greater equity for all.
In 2017, the Centers for Medicare and Medicaid Services (CMS) began adjusting star ratings for Medicare Advantage plans based on the level of service provided for those that have dual eligibility for Medicare and Medicaid which is a considered an indirect measure of socioeconomic status. Unfortunately, this measurement is not specific enough to understand their needs and adjust them accordingly.
A recent study by Durfey et al., published in Health Affairs, evaluated revisions in Medicare Advantage plans’ relative performance in three clinical quality measures after adjusting for selected widely available individual and area-level sociodemographic factors not included in CMS’s risk adjustment methodology. By adjusting for SES, the study found improvement in all three of the clinical quality measures. Therefore, their study suggested that including socioeconomic factors in the risk-adjustment models would lead to improved outcomes in those that are most disadvantaged.
If we are to deliver enhanced value to all we serve, we will need to grapple with the polarity of equity vs. equality as we have limited resources and the needs are vastly different. Let us continue the conversations on how to include SES not only in our treatment models but also in our risk stratification.
